Menu
Close
Back
Welcome to
Together is a new resource for anyone affected by pediatric cancer - patients and their parents, family members, and friends.
Learn MoreTotal lymphatic irradiation (TLI) is radiation therapy given to the lymphatic system. TLI uses high-energy x-rays. TLI is an important part of some stem cell (bone marrow) transplants.
The lymphatic system is part of your immune system. Normally, having a strong immune system is good. But the immune system can also attack the new, healthy donor cells your child gets in a transplant. TLI helps turn off the immune system for a short time, so it will not harm the new cells.
Doctors use chemotherapy and TLI together to prepare for the transplant. TLI may occur before, during, or after chemotherapy. It usually includes 4 doses.
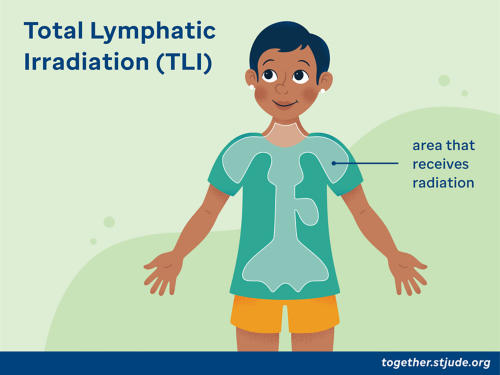
Total lymphatic irradiation (TLI) is radiation therapy given to the lympathic system.
About 1-2 weeks before TLI, you will meet with a radiation oncologist (a cancer doctor who specializes in radiation therapy). The radiation oncologist will explain TLI and discuss the benefits and potential side effects.
You will also meet other care team members. These include nurses, child life specialists, and radiation therapists (the people who give the TLI treatments). Your health care team will ask a parent or guardian to sign a consent form to give permission for TLI. The care team will let you know what to expect and answer your questions.
A simulation visit is a planning visit to help your child get ready for the actual treatment. During this visit, your care team will plan the radiation treatment and explain the process to you and your child. This visit can take up to 2 hours.
Your team will make a plastic mesh mask and a headrest to help your child stay in position during treatment. Then, your child will have a computed tomography (CT) scan in the treatment position.
A CT scan uses X-rays to create pictures of the inside of the body. The images from the CT scan will help plan the TLI treatment. Your doctor may use CT contrast for planning. The contrast highlights certain areas of the body to see them better on the CT scan.
During the simulation visit, your child will probably get 4-6 small permanent tattoos on the skin. These tattoos are about the size of a pencil tip, and they help mark the correct position for treatment.
The radiation therapist might also draw some lines on your child’s body with a marking pen. These are not permanent but help mark the correct treatment position. Please do not wash off these marks until your child is done with treatment.
Your child will not feel anything during TLI treatment. The machine might make a humming sound or other noises.
The radiation therapist will ask your child to lie on the radiation table using the mask and headrest. While receiving radiation, your child must be very still.
You may bring your child’s favorite music playlist or audiobook to play during the radiation treatments. Encourage your child to relax and breathe normally during treatment.
Your child will be alone in the treatment room during TLI when the machine is on. The radiation therapist will watch on the TV monitor and can see, hear, and talk to your child.
The total time for the TLI treatment is about 30 minutes. After treatment, there is no radiation in your child’s body or on their clothes. Your child is not radioactive and is safe to be around. Your child will go back to their hospital room after treatment.
Your child might have one or more of the side effects listed below. Because TLI is given as part of other treatments, it is hard to know if a side effect is caused by radiation, chemotherapy, or other treatments. Most side effects of TLI go away after treatment is over.
Side effects are called “early” or “late,” depending on when they happen after the start of treatment.
Early side effects can happen shortly after the start of TLI and up to 6 months after TLI ends. They include:
Late side effects can happen 6 months or longer after TLI. They can include:
Follow these tips to help take care of your child during TLI:
—
Reviewed: July 2022