Menu
Close
Back
Welcome to
Together is a new resource for anyone affected by pediatric cancer - patients and their parents, family members, and friends.
Learn MorePosterior fossa syndrome is also called cerebellar mutism syndrome. Children with posterior fossa syndrome may have problems with communication, motor skills, and mood. This syndrome sometimes develops after surgery to remove a brain tumor in the posterior fossa.
The posterior fossa is a space near the back of the base of the skull. It contains the cerebellum and brainstem.
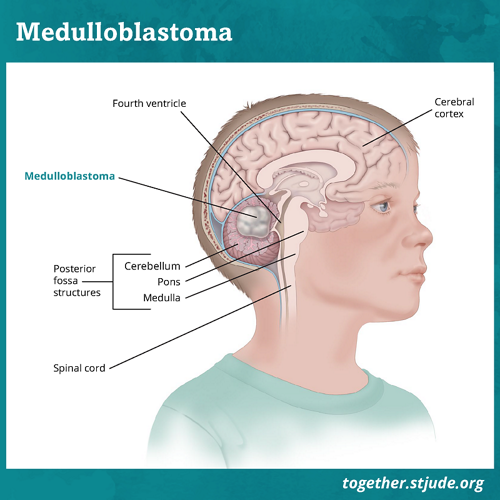
Tumors in the posterior fossa region account for over half of all brain tumors in children. About 25% of children who have surgery to remove medulloblastoma, a posterior fossa tumor, will develop posterior fossa syndrome.
Posterior fossa syndrome can happen after surgery to remove a brain tumor within the posterior fossa.
About half of all children’s brain tumors are in the posterior fossa. Medulloblastoma occurs in this part of the brain. It is the most common malignant brain tumor in children. About 25% of children who have surgery to remove medulloblastoma will develop posterior fossa syndrome.
But posterior fossa syndrome also can happen after surgery to remove other kinds of brain tumors in the posterior fossa. Those include astrocytoma and ependymoma.
Doctors do not know exactly why this condition affects some children and not others. The risk of posterior fossa syndrome is higher for children who are younger. This syndrome is also likely to occur when a child’s brain tumor:
Children with posterior fossa syndrome display 3 main types of symptoms:
Some children lose the ability to speak, also known as mutism. Other children can say a few words or speak only using short phrases.
Most children’s speech returns over the next few days or weeks. But some continue to have limited speech for months. Your child’s speech can sound different than it did before surgery.
Your child’s speech may improve over time. But some speech difficulties may not fully resolve.
Posterior fossa syndrome causes motor issues. These are the result of injury to the cerebellum.
A child with posterior fossa syndrome will have problems coordinating movements. This is known as ataxia. A child with ataxia will have trouble with large movements and/or fine motor skills such as:
Your child could have other motor difficulties including:
Children with posterior fossa syndrome often have problems controlling or expressing emotions.
They may show responses that are too exaggerated for the situation. They may be very irritable or agitated and cry often. But extra giddiness with unusual amounts of laughter can happen, too.
Children may have mood swings, or they may be difficult to calm. Your child may show little or muted response to things around them. This is often referred to as flat affect.
Mood changes may get in the way of your child’s ability or desire to take part in daily activities.
Symptoms of posterior fossa syndrome usually begin within 1–2 days after surgery. But symptoms always start within the first week after surgery.
Symptoms of posterior fossa syndrome range from mild to severe. Most children gradually improve and regain the ability to speak again. Most children will regain the ability to walk on their own. But some difficulties with speech, motor skills, and/or mood may last longer—even years.
If your child’s speech, motor, and mood symptoms begin to improve in the first week after posterior fossa syndrome begins, it is less likely they will have problems that require long-term help. It is more likely your child will continue to have problems that require help if it takes longer to show signs of improvement.
Therapies such as speech therapy can help to improve speech and swallowing difficulties.
Physical and occupational therapy can use motivating activities and exercise to improve your child’s ability to take part in self-care activities, to move, and to play on their own.
Working with a psychologist can help your child better manage moods and emotions. A neuropsychologist can work with your child to improve their thinking skills, such as:
Cognitive effects (issues with memory, attention, and decision making) are not used to diagnose posterior fossa syndrome. But they are common in children who have it.
Children with posterior fossa syndrome often have more problems with thinking skills and academic abilities. Some of these difficulties can take place as soon as 1 year after the brain tumor diagnosis. Other difficulties become more noticeable years later.
Your child may:
These difficulties are likely to persist to some degree.
Some children who have had posterior fossa syndrome will benefit from having formal academic accommodations in school.
Doctors may suggest a neuropsychological assessment (a test that can help measure attention, memory, language skills, decision making, and more). It can help identify patterns of strengths and weaknesses in a person’s thinking and academic skills. It can be used to recommend accommodations and modifications.
—
Reviewed: April 2023