Menu
Close
Back
Welcome to
Together is a new resource for anyone affected by pediatric cancer - patients and their parents, family members, and friends.
Learn MoreThe most common cause of pain in people with sickle cell disease is the sickling of red blood cells. When your child’s body is exposed to certain conditions, red blood cells containing hemoglobin S can become banana-shaped, hard, and sticky. These conditions can include:
As the hemoglobin releases oxygen, it causes the red blood cells to change from a normal round shape to an abnormal banana shape. This is also called a sickle shape.
The sickle-shaped red blood cells will stick together. They will clog tiny blood vessels and slow the delivery of blood and oxygen to the tissues.
Pain happens when the body’s tissues do not get enough oxygen. This is called an acute vaso-occlusion or pain crisis.
Keep in mind that your child may have pain that has nothing to do with sickle cell disease. Like everyone else, your child can get headaches, sprains, and other aches and pains that have nothing to do with sickle cell disease.
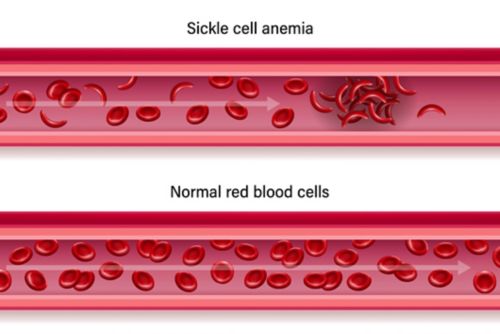
Acute pain in sickle cell disease can be related to clumping of sickle cells in veins and arteries
Pain crises (acute vaso-occlusive crisis) are the most common complication of sickle cell disease. The pain from this crisis is different from:
Pain related to sickle cell disease can happen at any time. Pain crises can keep your child from daily activities, like family time, meals, or school.
You can help your child manage mild to moderate pain at home. Severe pain needs to be treated by healthcare staff. Your child may need to be admitted to the hospital for pain control.
If your child is having a pain crisis, it’s important to get it treated as soon as you can. Treatment can reduce or control pain.
Acute pain crisis is the most common type of pain. It is unpredictable, comes on suddenly, and can occur without reason.
Pain severity varies, too. It could be mild, or it could be severe and debilitating. The pain can go from one part of the body to another part.
Acute pain can last for several hours to a few days. If your child has other health problems from sickle cell disease, the pain crisis can last for weeks.
Chronic pain is pain that is experienced on most days and lasts for 6 months or longer. It normally becomes more severe as people get older. More than 50% of adults with sickle cell disease experience chronic pain.
Assessing pain in sickle cell disease
When assessing acute and chronic pain, your child’s care team will want to know:
Your child will be asked to rate the pain on a pain scale if they are able. You can learn more about how your child’s care team measures pain here.
Pain treatments work differently for different people.
These tips can help you ensure your child is taking their prescribed medicines safely:
If the pain cannot be controlled or is severe, call your child’s care team.
Here are some things you can try with your child when they are dealing with pain. These techniques are not a substitute for pain medicine. But they can help the pain medicines work better.
| Technique | How it works | Examples |
|---|---|---|
| Relaxation |
|
|
| Distraction |
|
|
| Reframing/ Thought Stopping |
|
|
| Imagery/ Hypnosis |
|
|
| Modeling |
|
|
| Heat |
|
|
Contact your child’s care team if you have questions about pain.
—
Reviewed: August 2022