St. Jude continues to chart progress in how to understand and treat sickle cell disease
Pioneering work in St. Jude labs provides "promising" path to a cure using gene editing.
October 03, 2022 • 4 min

Nytasha was worried when the nurses whisked away her daughter moments after she was born. They said the baby was anemic and had jaundice. There could be something wrong with her liver.
But a blood test soon revealed Nytasha’s daughter, Za’Mya, was born with sickle cell anemia, one of the most common inherited blood disorders in the United States. About one out of 365 African American babies born in the U.S. has sickle cell disease — a genetic blood disorder found most commonly in the U.S. in individuals of African descent. Hispanic Americans and people of Mediterranean, Indian and Middle Eastern descent can also be affected.
Za’Mya, who is now 7, was diagnosed in the first week of her life and was referred for care and treatment at St. Jude Children’s Research Hospital, which runs one of the largest sickle cell programs in the country, treating about 900 children a year.
Nytasha was aware she carried the sickle cell gene, but knew little about the disease, which forms hard fibers inside red blood cells causing them to distort from healthy, round and plump into sickle or banana shapes. The abnormally shaped red blood cells cannot move through blood vessels easily, so they get stuck, preventing the crucial delivery of oxygen to some organs and tissues and causing debilitating, sometimes life threatening, pain crises.
For Za’Mya, the pain comes unexpectedly and throbs along her legs, but sometimes in her chest, too, forcing the family to rush to the hospital for urgent treatment.
She's very strong for her to be so young and going through what she goes through. She makes me brave.
“You know, she rarely cries, even though I know she's hurting like crazy,” Nytasha said. “She's very strong for her to be so young and going through what she goes through. She makes me brave.”
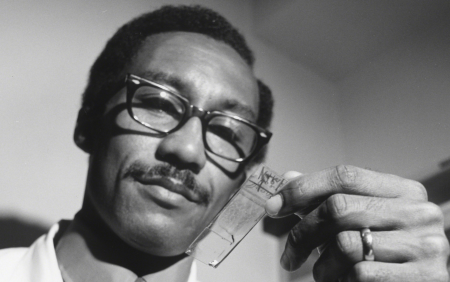
Over the last 60 years, doctors and researchers at St. Jude have set the stage to dramatically improve the care and understanding of sickle cell disease.
It was on this campus in Memphis where an African American doctor, Rudolph Jackson, developed community outreach programs and clinical protocols serving sickle cell-affected families in 1968. In a few years, Jackson’s pioneering work had amassed such recognition and stature that the federal government asked him to help establish a national protocol for the treatment and care of sickle cell patients.
A St. Jude patient was the first in the world to be cured of sickle cell anemia through a stem cell/bone marrow transplant. And work led by scientists and researchers at St. Jude also showed that using the drug hydroxyurea daily could boost average hemoglobin levels, thus severely reducing the frequency of hospitalization for pain crises.

Recently, St. Jude partnered with other top institutions in the country through its Research Collaboratives program to develop and refine novel gene therapies that would allow doctors to edit the genes responsible for sickle cell in fetuses, allowing babies prone to the disease to be born healthy. Published early results of gene editing studies are “very promising,” said Dr. Clifford Takemoto, Director of Clinical Hematology at St. Jude and Lemuel Diggs Endowed Chair in Sickle Cell Disease.
St. Jude also recently opened a telehealth clinic for sickle cell disease patients in Tupelo, Miss., helping patients who live too far from the main campus in Memphis to easily attend appointments.
Still, there is much work left to do to improve the lives of the more than 100,000 patients affected by sickle cell in the U.S., and the tens of thousands with it around the world, particularly in Africa, Takemoto said.
“I will say that there has been progress made in terms of understanding and knowing that if we give something very simple like penicillin to babies, that infants that used to die early on, that doesn’t happen anymore, so that is much better and children are living and doing well,” Takemoto said.
Takemoto added that other screening measures have also been developed that identify children at risk for other major life-threatening conditions such as stroke. So now, therapies can be be implemented before children experience such devastating complications. Using these new therapies and screenings, doctors and scientists have markedly reduced the chances of early death and disease caused by sickle cell. That is, until adulthood.
"That’s where things have not changed much,” Takemoto said, stressing the need for continued research in this area. “This is a condition where the life expectancy is still in the mid-40s.”

Dr. Clifford Takemoto, Director of Clinical Hematology at St. Jude.
These realities weigh on Nytasha’s mind. She asks lots of questions at clinic visits about Za’Mya’s prognosis, which looks encouraging now, and has enrolled her older sons in trials at St. Jude so they will know more about the disease for which they carry a gene when it comes time for them to have children.
Recently, she brought Za’Mya to the St. Jude campus to meet the crew members of a new space mission to benefit the research hospital. The 7-year-old was shy with the astronauts as they asked her questions, but proudly showed them a rocket she painted in vibrant pinks and yellows.
Sitting there, surrounded by folks talking about the stars and heavens, Nytasha couldn’t help but share what she dreams for her daughter.
“She's going to get married. She's going to have me some grandbabies. We are going to take trips. She’s going to be a doctor. She's going to do everything she wants to do…and more,” Nytasha said.