St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Stephen Gottschalk Lab
Exploring translational immune-oncology and immunotherapy for pediatric cancer
About the Gottschalk lab
The immune system acts as the body’s defense mechanism against disease and infection. However, cancers have developed multiple mechanisms to evade immune recognition, which makes it difficult for the immune system to eradicate cancer. Our laboratory’s goal is to develop genetic approaches to help the immune system provide cures for currently “incurable pediatric cancers.” Our research applies directly to the treatment of pediatric patients, and this translational aspect of our laboratory is one that drives new discoveries for treatments of children with catastrophic diseases.

Our research summary
Our laboratory focuses on translational immuno-oncology and immunotherapy for pediatric cancer. Adoptive immunotherapy with T cells, genetically engineered to express chimeric antigen receptors (CARs), has been highly effective for B-cell acute lymphoblastic leukemia (ALL) and lymphoma, leading to approval by the US Food and Drug Administration (FDA). However, CAR T cell therapy approaches have shown limited antitumor activity for solid tumors and brain tumors.
This lack of efficacy is most likely multifactorial, including a limited array of targeted antigens, and the inability of CAR T cells to sustain their effector function in the tumor microenvironment. Most existing CAR T cell therapy approaches have only targeted cancer cells—not cells of the tumor stroma—which play a critical role in promoting tumor growth and therapeutic resistance.

Collaboration is a key component in our work to overcome the limitations of CAR T cell therapy, and we employ a collaborative approach with the Department of Bone Marrow Transplantation and Cell Therapy (BMTCT). Other collaborative efforts include projects with the Departments of Immunology, Computational Biology, Pathology, and Chemical Biology and Therapeutics (CBT).
As we focus on immune cells’ ability to sustain their effector function in the setting of chronic antigen exposure, we employ genetic engineering approaches. We explore transgenic expression of native and synthetic molecules as well as the deletion of negative regulators to prevent immune cell differentiation into a dysfunctional state.
To enhance therapeutic efficacy, we study combinatorial approaches in which engineered immune cells combine with other therapeutic modalities. While the bulk of our work concentrates on CARs, we actively examine other approaches to make cancer-specific immune cells. For our immunotherapy approaches, we explore T cells and natural killer (NK) cells as immune effectors.
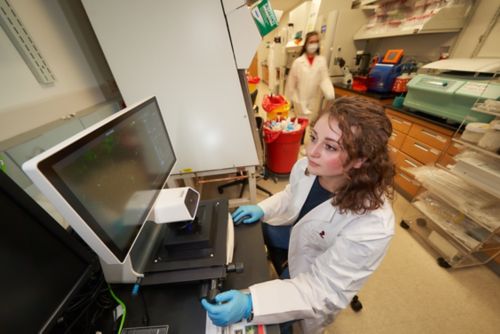
A wide array of approaches, including 2D and 3D cell culture systems, flowcytometry, advanced imaging, and singe cell analysis allows us to evaluate the function of engineered immune cells. For our in vivo studies, we take advantage of cell line xenograft, patient derived xenograft (PDX), and immune competent syngeneic models.
Once we select a cell therapy approach for clinical evaluation, we work closely with our Clinical Research Office, the Regulatory Affairs Office, the Experimental Cellular Therapeutics Laboratory, and the Children’s GMP to translate our approach into early phase clinical testing. Our expansive and collaborative research strategy ensures our laboratory can advance translational immune-oncology and immunotherapy for pediatric cancer.
Publications
Contact us
Stephen Gottschalk, MD
Member, St. Jude Faculty
Department of Bone Marrow Transplantation & Cellular Therapy
MS 321, Room I4112
St. Jude Children's Research Hospital
Memphis, TN, 38105-3678 USA GET DIRECTIONS

