St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Mack Lab
Deciphering epigenetic and transcriptional mechanisms of cancer through the lens of pediatric brain tumors
About the Mack Lab
Pediatric brain tumors are the leading cause of cancer-associated death in children. Understanding the origins and mechanisms of these diseases is central to developing new treatment approaches. Our lab is interested in interrogating the epigenetic and transcriptional landscape of pediatric brain tumors and translating these findings into the clinic. We hope to improve our understanding of general principles of cancer, while creating rational and effective solutions for our patient populations.

Our research summary
Our lab is interested in pediatric brain tumors with a focus on ependymoma, a devastating cancer arising from the ventricular system. We use state-of-the-art technologies to ask critical questions and explore fundamental mechanisms regulating disease origin, development and response to therapy. Through clinical and research collaborations, we identify biologically relevant and actionable targets and test candidate therapeutics in a comprehensive preclinical pipeline.
Epigenetic landscape alterations in pediatric brain tumors
Epigenetic regulators and fusion proteins are drivers in cancers like ependymoma and high-grade glioma. We are interested in deciphering alterations to transcriptional landscape and chromatin architecture with a focus on K27M-driven high-grade gliomas and RELA fusion ependymoma.
Our team uses in utero electroporation of cancer drivers to transform cells during development to generate animal models of these diseases. Our research approach utilizes bulk and single cell sequencing approaches to characterize transcriptional programs and epigenetic landscapes. We also utilize compound and genetic screening to dissect mechanisms of these cancer drivers on the epigenome.
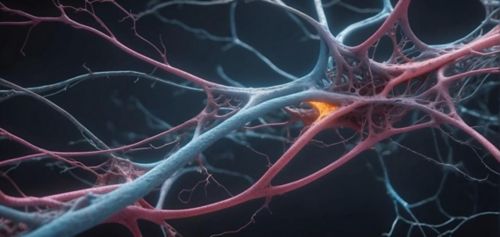
Biomolecular condensates of DNA-binding fusion oncoproteins
Recent work suggests that RELA fusion proteins regulate nuclear condensates, self-organizing suborganelle compartments that regulate the interactions between genomic DNA and transcriptional machinery. Transcriptional phase condensates are emerging as an important regulator of gene expression and driver of disease, although mechanisms are largely unknown. We are studying the how components of fusion oncoproteins contribute to pathological, novel functions by testing bioinformatics predictions with targeted mutagenesis and synthetic genetic constructs. This has stimulated a new project pipeline to explore phase separation and its role in tumorigenesis by combining structural biology, biophysics, genetics and molecular biology.
Interactions between tumor and microenvironment
We have identified neuronal activity increases tumor development in ependymoma by the neurotransmitter serotonin directly binding tumor cell histones. Serotonin binding regulates the epigenetic landscape and alters the expression of transcription factors and neuropeptides that drive tumor growth.
By modeling ependymoma by electroporating fusion oncoprotein drivers, we can integrate cancer biology with state-of-the-art viral tracing, genetic and imaging approaches for studying cancer neuroscience. We are interested in characterizing connections between neurons and tumor cells and molecular factors driving the pathological positive feedback loop between neuronal activity and tumor growth.
Targeting molecular findings to clinical applications
Recognizing the need for new targeted therapies, our team has developed an extensive network of collaborators to design and evaluate interventions. We partner with clinicians to determine clinical priorities and opportunities and design robust preclinical studies to inform future development. We have generated the largest set of patient-derived ependymoma samples and models to evaluate tumor dependencies with functional in vivo screens.
Ongoing projects include developing compounds to correct epigenetic changes in pediatric cancers and identifying cell surface antigens for designing and improve CAR-T based therapies. We are investigating whether the process of forming condensates is druggable and how phase separation may interact with drug delivery.
We are also exploring opportunities for combination therapeutic approaches slowing tumor pathogenesis by targeting extrinsic signaling to disrupt interactions between the epigenetic landscape and tumor environment. Through partnerships with clinical trials at St. Jude, we hope to deliver these preclinical findings to improve patient outcomes and care.
Selected Publications
Contact us
Stephen Mack, PhD
Associate Member
Department of Developmental Neurobiology
MS 323, Room M3405
St. Jude Children's Research Hospital
Follow Us

Memphis, TN, 38105-3678 USA GET DIRECTIONS