St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
About the McKinney-Freeman Lab
Hematopoietic stem cells (HSCs) are often exploited for therapeutic use. Dysfunction of this cell population lies at the heart of hematological disease. Our laboratory explores the fundamental biology of HSC ontogeny, molecular regulation, and transplantation. This work will illuminate underlying mechanisms of disease. We hope to reveal potential opportunities to improve transplantation-based therapies.

Our research summary
Hematopoietic stem cells (HSCs) are routinely used to treat leukemia and hematologic disease through HSC transplantation therapies. Many patients who would benefit from this form of therapy, however, lack access to a suitable donor. Our laboratory explores the fundamental biology of HSCs, particularly the genetic and cellular regulation of their in vivo repopulating activity. By better understanding the factors controlling the ability of HSCs to home to, engraft, and repopulate the hematopoietic compartment after transplantation, we hope to develop better and more effective HSC transplantation therapies.
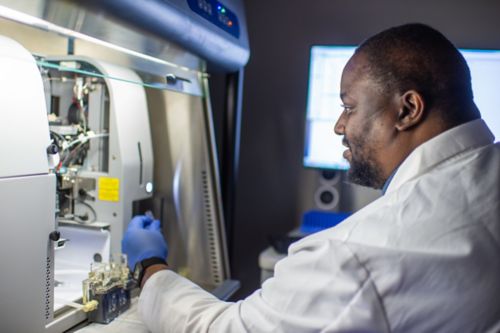
The projects in our laboratory explore HSC ontogeny, the molecular regulation of HSC transplantation, and the effect of chronic hematologic stress and disease on these stem cells. Our work incorporates several approaches and techniques, including flow cytometry, fate mapping, functional studies, single-cell RNA sequencing, bioinformatics, imaging and pathology.
HSC ontogeny
In this line of investigation, our laboratory aims to better understand the precise way in which HSCs emerge during embryogenesis and how the hematopoietic hierarchy is established in the bone marrow during fetal and early life. Recently, we have isolated HSC populations of interest across the entire course of mammalian development – from mid-gestation through four weeks of age – to take a deeper look at the heterogenicity of the bone marrow niche and the HSC pool across this relatively unexplored window of HSC ontogeny. Using novel fate-mapping technologies, we are able to apply a bioinformatics-based approach to analyze cell populations during early development and across lifespan.
Molecular regulation of HSC transplantation
Another area of research in our laboratory focuses on the molecular regulation of HSC following transplantation. Using an unbiased screening approach, we identified a large number of putative genetic regulators previously unidentified in the context of HSC biology. From this screen, we have prioritized multiple candidates for follow-up studies using mouse models and molecular approaches to illuminate precisely how they control HSC function. We are now translating our discoveries to human HSC and leveraging them to enhance HSC transplantation, especially in contexts where HSC engraftment is compromised (e.g. hematopoietic disease). Increasing our understanding of engraftment regulation, we envision robust collaboration with the Department of Chemical Biology and Therapeutics to explore small molecule-based interventions for improved transplant efficiency.

HSC and Hematologic Disease
Our laboratory also studies how chronic hematologic stress or chronic hematologic disease corrupt HSC function. We are specifically focusing on sickle cell anemia (SCA), using both mouse models of the disease as well as clinical samples to see how the fitness of the HSCs is compromised in this disease setting. Towards this work, we have developed key partnerships with scientists and clinicians here at St. Jude and in local adult hospitals. Looking ahead, our laboratory seeks to identify the molecular pathways that are perturbed in SCA HSCs and develop strategies to rejuvenate these dysfunctional HSCs, which will benefit cell-based therapies for these patients that depend on their HSCs.
Selected Publications
Contact us
Shannon McKinney-Freeman, PhD
Member
Department of Hematology
MS 341
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS