St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Charles J. Russell Lab
Studying respiratory viruses to develop and optimize effective vaccines and therapeutics
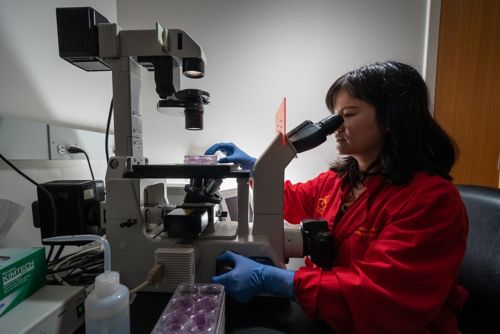
About the Russell lab
The emergence and evolution of viral pathogens creates an ever-changing infectious disease landscape throughout the world. But as pathogens emerge and shift, so does technology. Our laboratory leverages cutting-edge research technology to study respiratory viruses at the bench, which we then translate to the clinical setting. The breadth of our work allows us to contribute to the collaborative development of vaccines and therapeutics designed to elicit an enhanced immune response against respiratory viruses in healthy and immunocompromised individuals.

Our research summary
The study of respiratory viruses hinges upon the ability to study the emergence and evolution of viral pathogens and subsequently develop vaccines and therapeutics that aid in infectious disease management.
The root of our work begins with an understanding of how viruses enter host cells and cause infection. To deepen our understanding of viral infection, replication, and transmission mechanisms, our laboratory concentrates on envelope surface glycoproteins. Our research in this area extends to vaccine development and allows us to engage in many collaborative efforts. Beyond glycoproteins and vaccine development, we concentrate on viral infection in immunocompromised individuals and how best to optimize therapeutic treatments in this population.
Envelope surface glycoproteins
In our study of RNA viruses, we focus on the role of envelope surface glycoproteins. Because RNA viruses are membrane-bound viruses, they have a cellular envelope from which proteins protrude. These protruding glycoproteins bind to, and fuse with, the host cell membrane so a virus can center a cell.
Because of the functional role of these proteins, we study their structure, role in viral entry, and how mutations can lead to infection and transmission across species. Our work allows us to deepen our understanding of the particular role glycoproteins play and explore how we can engineer and leverage these proteins in vaccine development.
Vaccine development
Our understanding of envelope surface glycoproteins extends to our collaborative work in vaccine development. We partner with the Hurwitz laboratory in the Department of Infectious Diseases to leverage our knowledge of these proteins in the development of a Sendai virus vector that targets parainfluenza virus type 1 (PIV1)—the cause of croup in babies. With this vector, we create vaccines against other respiratory viruses like RSV, PIV3, and human metapneumovirus. This work is particularly exciting as the National Institutes of Health (NIH) is currently testing the vaccine in humans, and our partnership with the Serum Institute of India enables us to plan for large-scale clinical trials.
In another area of our vaccine-development work, we examine the influenza hemagglutinin protein and how we can stabilize its structure to improve flu vaccinations. We also examine hemagglutinin receptor binding and stability to discern what role these processes and properties play in species-dependent infection and transmission (avian, swine, or human).
Our laboratory is also involved in collaborative research concerning the mRNA platform for vaccine development, which holds significant promise and excitement.

Luciferase infection models
To examine viral infection in immunocompromised hosts and examine potential therapeutic treatments, we employ luciferase infection models. With the luciferase infection models, we can examine chronic, long-term infections via noninvasive bioluminescent imaging. We start with a bioluminescent paramyxovirus or a bioluminescent influenza virus and then induce an immunocompromised state that mimics a chemotherapeutic response in our experimental model. We study the kinetics and dynamics of the infection over time, which offers insight as to when we can best introduce treatment during infection. The use of luciferase infection models also allows us to evaluate which treatments are most effective to counteract an infection.
We are currently evaluating the use of a new drug—a polymerase inhibitor—to treat influenza in immunocompromised experimental models. We hope to discover whether the infection rebounds at a later point in time so we can help devise a better therapeutic strategy. The goal of this work is to uncover a general notion of what infection looks like in immunocompromised individuals and what we can do to optimize treatment.
Because of the innovative environment and access to cutting-edge resources at St. Jude, our laboratory can expand beyond the study of one step in the virus replication cycle. We can look at viral infectious diseases in experimental models and conduct translational, collaborative work that contributes to ongoing vaccine development.
Publications
Contact us
Charles J. Russell, PhD
Associate Member, St. Jujde Faculty
Department of Host-Microbe Interactions
MS 330, Room I6309
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS