St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Wilson Clements Lab
Investigating how the adult blood and immune systems are specified during embryonic development
About the Clements Lab
Hematopoietic stem cells (HSCs) are the foundational unit of the adult blood and immune systems. They are the therapeutic component of bone marrow transplants, used in the treatment of hematological and autoimmune disorders. Our laboratory is committed to understanding the molecular, cellular, and extracellular context in which HSCs are specified. The discoveries we make will inform disease mechanisms and improve therapies.
Our research summary
Hematopoietic stem cells (HSCs) arise from endothelial cells found in the primitive descending aorta of mammals or the dorsal aorta of anamniotic vertebrates such as zebrafish. We are interested in understanding the basis of regulation of induction of hematopoietic potential, maintenance of “stemness,” control of proliferation, and mobilization of migratory behaviors. In the long term, we hope that by understanding the basis of regulation of these behaviors we can harness them usefully for directed differentiation and to understand their dysregulation in disease such as leukemia.
Why HSCs?
HSCs are the fundamental unit of the hematopoietic system, which provides all red and white blood cells of the body throughout life. They both self-renew and give rise to daughter cells that have the capacity to proliferate and differentiate into the effector cells that carry oxygen to all tissues of the body, heal wounds, regulate inflammatory responses and fight invading pathogens. Clinically, HSCs are used in transplant therapies for disease, most notably leukemia, but now in a growing number of nonmalignant hematologic diseases, including hemoglobinopathies such as sickle cell disease, congenital neutropenias, and autoimmune disorders. Understanding the physiological basis of HSC specification is conceptually the first step in attempting to reproduce that process for in vitro directed differentiation of HSCs for clinical use.
The specification niche
HSCs are born from transient endothelial precursor cells in the major thoracic arterial vessel of vertebrates. This population of cells, termed “hemogenic endothelium,” is a uniquely competent tissue programmed to be able to receive and integrate myriad signals that converge to direct HSC specification. The complex local microenvironment, composed of cells, circulating primitive blood and extracellular matrix, provides these essential cues to transform hemogenic endothelial target cells into the first definitive hematopoietic stem and progenitor cell precursors, which will migrate to subsequent maturation, expansion and residency tissues. Decades of research have uncovered numerous critical signals that direct this transformation, but the impossibility of recapitulating HSC specification in vitro indicates that additional signals remain to be uncovered. We hypothesize that these signals live in the local microenvironment and are provided by neighboring cells in the mesenchyme and adjacent nonhemogenic endothelium. Our previous research showed that neural crest (Damm and Clements, Nature Cell Biology, 2017) and sclerotome are key cellular neighbors that direct HSC outcomes. We are now working to determine the signals or other mechanisms by which these niche cells regulate HSC specification. More recently, we have determined that the physical properties of the local environment, such as noncellular matrix molecules and stiffness, likely contribute to the overall effectiveness of HSC emergence.
Our models
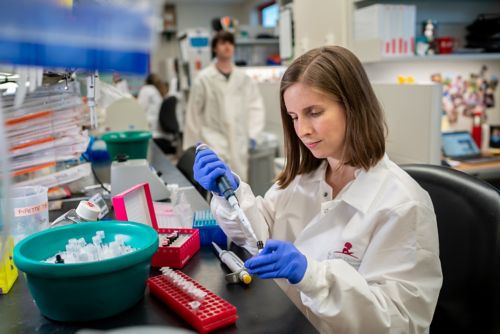
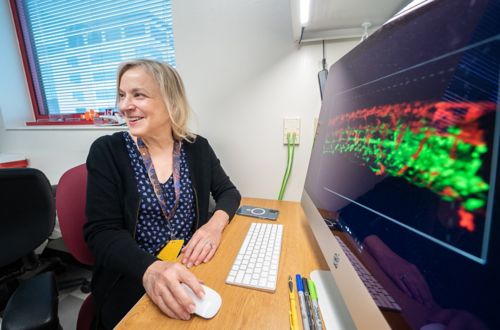
The Clements group uses parallel vertebrate models to realize complementary strengths and speed investigation. Our primary discovery model is the zebrafish embryo, which overwhelmingly shares genetic regulation of hematopoietic development, homeostasis and disease with humans. Zebrafish have cognates of all mature human hematopoietic lineages, and embryos are transparent, allowing direct observation of tissue development by fluorescence and traditional light microscopy, as well as being highly receptive to transient and genetic gain and loss of function approaches. We use mouse as a mammalian validation platform and to be able to perform transplant and in vitro colony formation assays.
Our future
Identification of required HSC specification niche cell populations has allowed us to use multiple complementary strategies to identify novel peptide, small molecule and biophysical contributions to HSC specification. We are using single-cell RNA-seq and spatial genomics to identify hidden populations within our niche cells, while in parallel performing deep transcriptional profiling to uncover previously unknown peptide signals, metabolic/synthetic enzymes and modifiers of physical geography that control hematopoietic development. In the long term, we seek to integrate novel regulatory mechanisms into existing directed differentiation protocols to achieve high efficiency in vitro specification of HSCs with normal self-renewal and lineage maturation capabilities.
Selected publications
Contact us
Wilson K. Clements, PhD
Associate Member, St. Jude Faculty
Hematology
MS 355
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS