St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Preclinical Design and Development Core
Driving variant-to-therapy translation for ultrarare genetic diseases
About the Core

The Preclinical Design and Development (PDD) Core is a translational research lab housed within the Pediatric Translational Neuroscience Initiative (PTNI)’s Center for Pediatric Neurological Disease Research (CPNDR). The PDD Core employs a modular and scalable preclinical pipeline for development of potential individualized genomic therapies for patients enrolled in PTNI’s Blue Sky Initiative GEMINI program.
The PDD Core’s current focus centers on antisense oligonucleotides (ASOs), a promising class of RNA-targeted therapies designed to modulate gene expression in a mutation-specific manner. Through a streamlined workflow, the PDD Core designs, tests and validates therapeutic lead candidates in vitro, laying the groundwork for future clinical translation. The PDD also performs in vitro studies to establish the molecular consequences of a genetic variant and to identify strategies for developing, testing and validating potential therapeutic candidates.

Impact
Developing therapeutics for children with ultrarare diseases is not considered commercially viable and thus lies outside the scope of traditional pharmaceutical companies. Through the GEMINI program, St. Jude brings innovative precision medicine approaches into the clinic to treat patients with neurological disorders, thus establishing St. Jude as a foundational leader in addressing this critical unmet need for catastrophic pediatric neurological diseases.
The PDD Core works to develop, operationalize and optimize the ASO development pipeline at St. Jude. By integrating patient-derived models with targeted molecular design and comprehensive screening efforts, preclinical development of therapeutic candidates can be tailored to the patient’s genetic profile. This process is designed to bridge the gap between genetic diagnosis and therapeutic intervention, supporting the GEMINI program’s broader mission to deliver individualized treatments.
Core capabilities
Patient-Derived Models
Establishment of disease-relevant cellular models from patient biospecimens to enable functional testing
Integrated Sequencing Analysis
Validation of pathogenic variants and their downstream molecular consequences using long- and short-read multi-omic profiling to inform therapeutic strategy
ASO Design
Rational design of ASOs for splicing correction or RNA modulation, tailored to variant-specific mechanisms
Functional Evaluation
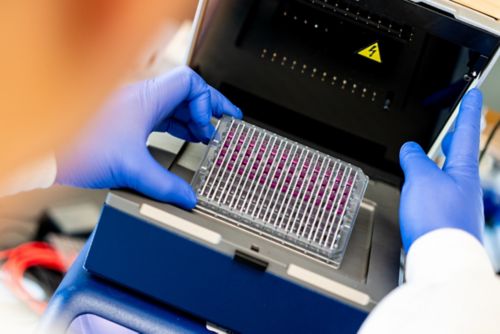
High-throughput screening of candidate ASOs in patient-derived models to assess transcript modulation efficacy and identification of lead candidates
Safety Assessment
In vitro toxicity profiling of lead candidates to support advancement towards clinical translation
Process Flow Development
Development of process flows for preclinical manufacturing integration
Automation

To increase throughput and improve reproducibility, the PDD Core is implementing an automated liquid handling system to support functional screening of antisense oligonucleotides (ASOs). This transition is enabled by advanced high-throughput robotic platforms, including the JANUS G3 Expanded systems (8-tip + MDT, RUO; and MDT, IVD configurations), which collectively support scalable processing of more than 500 oligonucleotide candidates per patient-derived cell line. This automation enhances assay consistency, reduces manual variability and enables systematic expansion of individualized RNA therapeutic development across a growing number of cases.
Patient-derived cell models
-
Slide activated
Fibroblast derivation from patient biopsy.
-
Slide activated
NGN2-derived neurons with MAP2 staining (image credit: Mefford lab).
-
Slide activated
iPSC-derived neurons with MAP2 and FOXG1 staining (image credit: Mefford lab).
About the director

Dr. Rachayata Dharmat received her PhD from Baylor College of Medicine (BCM), where she trained in cell and molecular neurobiology, mouse genetics and neural development with an emphasis on neurological disease. Before leading the PDD Core, she was a postdoctoral fellow with Dr. J. Paul Taylor in the Department of Cell and Molecular Biology. Dr. Dharmat has expertise in neurological disease modeling, gene discovery and functional genomics, with a strong interest in developing therapeutic approaches for neurological disorders. From her role as an initial team member at the BCM Single Cell Genomics Core, she has expertise in establishing core standard operating procedures (SOPs) and providing high-quality research support. As director of the PDD Core, Dr. Dharmat is establishing the preclinical pipeline for the development of individualized genomic therapies through the St. Jude Pediatric Translational Neuroscience Initiative’s GEMINI program, initially focusing on antisense oligonucleotides.
The team
- Mohamed Ghonim, PhD
- Scientist

- Asmita Ghosh, PhD
- Scientist
Contact us
Rachayata Dharmat, PhD
Center for Pediatric Neurological Disease
MS 326, Room M3345
St. Jude Children Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS


