St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
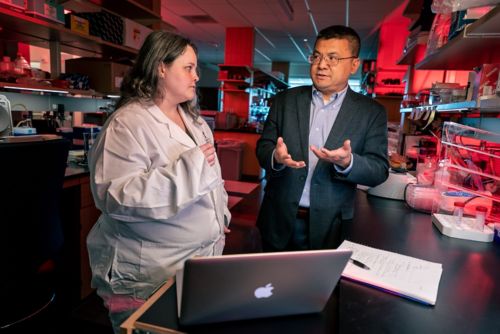
Hongbo Chi Lab
Investigating immune cell metabolism (immunometabolism) in adaptive immunity and immunotherapy by integrating systems biology and functional genomics with immunology
About the Chi Lab
Cellular metabolism is connected to immune responses and diseases such as cancer. Our laboratory seeks to understand how these connections work by applying systems biology and functional genomics tools and interdisciplinary strategies. We aim to gain new insights into immunobiology and disease mechanisms and discover actionable therapeutic targets.

Chi Lab research summary
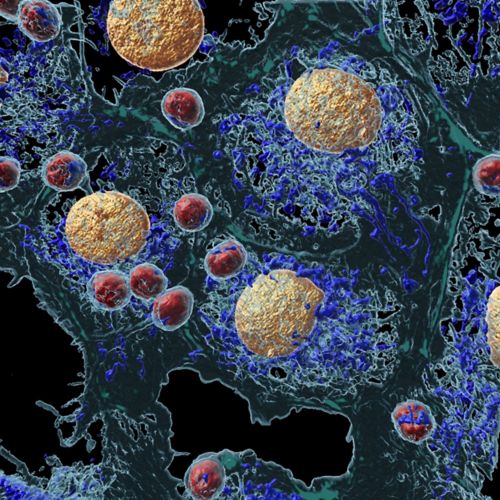
Metabolism is the core process underlying all biological functions. Our goals are to discover the mechanisms linking the metabolic state of immune cells (immunometabolism) with tissue homeostasis and function, and to use these insights to develop better treatments for cancer and other diseases.
We are particularly interested in understanding metabolic programs, mTOR and nutrients (Signal 4), and systems-level regulatory networks in basic T-cell and dendritic cell biology and antitumor immunity. To gain an integrative view, we combine the traditional hypothesis-driven approach with systems biology principles, especially in vivo CRISPR-based functional genomics screens, to identify new concepts and hidden drivers for immunometabolism that cannot be surmised from simpler systems or the “reductionist” approach. Our research program addresses the following fundamental questions in immunometabolism and systems immunology:
Metabolic reprogramming of cell fate: Our laboratory has a long-standing interest in understanding metabolic programs and adaptation underlying immune cell fate and function. We discovered critical roles of glucose, lipid, amino acid and mitochondrial metabolism in cell fate choices between effector (e.g., Th17 and Tfh), regulatory and memory T cells, as well as context (e.g., tissue or tumor microenvironment)-specific metabolic adaptation and heterogeneity. Beyond T–cell-intrinsic metabolism, our laboratory established the metabolic dependence of dendritic cell subsets as a key extrinsic mechanism that regulates T cell responses, including the selective roles of mitochondrial and glutamine metabolism in type-I dendritic cells (cDC1) for anti-tumor immunity.
mTOR and nutrient signaling: Our laboratory contributed to the emerging concepts of T-cell metabolic quiescence and quiescence exit, and nutrients as “Signal 4” to license T-cell activation. In particular, we discovered that mTOR signaling is a rheostat for T-cell quiescence versus quiescence exit, and uncovered three-tiered modules of nutrient signaling encompassing nutrient transporters, sensors, and transducers that mediate mTOR activation and T-cell responses. In addition to mTOR signaling, we investigate other nutrient-related signaling pathways, including LKB1, folliculin, Hippo, and autophagy.
In vivo CRISPR screens and systems immunology: We apply high-throughput in vivo CRISPR functional screens to discover novel metabolic checkpoints and causal networks. Our in vivo functional genomics approaches identified new targets to reprogram T-cell anti-tumor functions and overcome tumor immune evasion. Our in vivo single-cell CRISPR screens enabled the reconstruction of causal networks and cell fate regulomes. Moreover, we developed and advanced multi-omics systems tools in immunology, including systems proteomics and data-driven network approaches to infer protein activity (hidden drivers).
Immunometabolic engineering and therapeutic translation: Capitalizing on the remarkable expertise of St. Jude in pediatric cancer research and treatment, we use functional genomics and systems immunology strategies to identify actionable disease targets in pediatric immuno-oncology, by exploiting the metabolic barriers to immunity and disease. This new frontier in our research program involves extensive collaborative efforts, exemplified by an interdisciplinary initiative to identify innovative immuno-oncology targets in pediatric cancer, known as the iTARGETS (Immuno-Oncology Target Identification via Systems Immunology) “blue sky” project. Moreover, efforts are underway to engineer next-generation CAR T cells (e.g., by editing the REGNASE-1 gene) for clinical translation for pediatric cancer therapies.
By integrating hypothesis-driven and systems immunology approaches, we will establish fundamental insights into immunometabolism and adaptive immunity and discover the mechanisms and targets that connect metabolic programs to immunity and disease.
Find out more
Immunity in the spotlight: how vaccinations and the immune system protect us
Researchers at St. Jude explain what immunity is and how it works.
Understanding the complex networks behind a functional adaptive immune system
Explore how a T cell knows what it is, and what to do, through research happening at St. Jude.
Contact the Chi Lab
Hongbo Chi, PhD
Chair, Department of Immunology
MS 351, Room M5424
St. Jude Children’s Research Hospital
Follow us

Memphis, TN, 38105-3678 USA GET DIRECTIONS






