St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Solving the decades-long mystery of NLRC5 sensor function in inflammation and disease
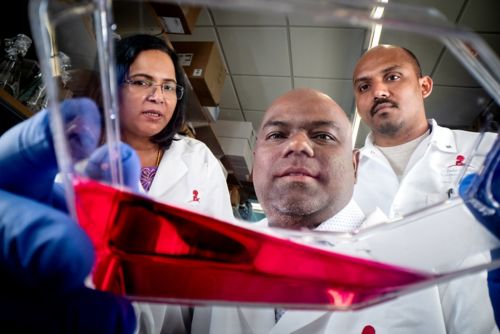
Thirumala-Devi Kanneganti, PhD; Balamurugan Sundaram, PhD; and Nagakannan Pandian, PhD, Department of Immunology, published research revealing the function of the innate immune sensor NLRC5 in cell death.
Innate immune sensors are an integral part of the immune system, acting as a first line of defense to protect against disease and infection. Activated sensors trigger a cascade of events that can be beneficial and provide host defense but can also cause inflammation and disease.
As part of their response, innate immune sensors assemble complexes that integrate signals and respond to threats. One such complex is the PANoptosome, which drives a prominent inflammatory cell death type called PANoptosis. However, how specific innate immune sensors work and what triggers them to act have remained mysterious for decades.
Chipping away at the mystery, scientists at St. Jude, led by Thirumala-Devi Kanneganti, PhD, Center of Excellence for Innate Immunity and Inflammation director and Department of Immunology vice chair, published research in Cell showing how a member of the nucleotide-binding oligomerization domain-like receptor (NLR) family, NLRC5, plays a previously unidentified role driving PANoptosis.
To understand its role in disease and elucidate the triggers of NLRC5, the scientists screened combinations of immune-system threats, including pathogen-associated molecular patterns (PAMPs), damage-associated molecular patterns (DAMPs), and cytokines (immune signaling molecules) that can be released by or mimic an infection, injury, or illness. This comprehensive approach is built on extensive research that has shown the multifaceted nature of innate immunity; this contrasts with the conventional single ligand-receptor model of study, which has historically oversimplified the complex interplay of innate immune signaling.
Through this process, the researchers examined heme, a hemoglobin component that binds oxygen to carry the molecule throughout the body. However, “free heme” can also be released when red blood cells rupture, leading to inflammation and organ damage.
“We identified that the combination of heme plus PAMPs or cytokines specifically induces NLRC5-dependent PANoptosis,” said co-first author Balamurugan Sundaram, PhD, Department of Immunology. “This showed for the first time that NLRC5 is central in responding to hemolysis, which can occur during infections, inflammatory diseases, and cancers.”
The results led the team to investigate how NLRC5 is regulated. They found that depletion of a key molecule for cellular energy production — nicotinamide adenine dinucleotide (NAD) — signals to the immune system that there is a threat, driving NLRC5 protein expression.
“Supplementing with the NAD precursor, nicotinamide, blocked NLRC5-mediated PANoptosis,” said co-first author Nagakannan Pandian, PhD, Department of Immunology. “Therapeutically, nicotinamide has been used as a nutrient supplement, and our findings suggest it could help treat inflammatory diseases.”
With this knowledge, the team searched for how NLRC5 could be a target in therapeutic approaches to mitigate PANoptosis associated with diseases. They found that deleting Nlrc5 protected against inflammatory cell death and prevented disease pathology in hemolytic and inflammatory disease models, making NLRC5 an exciting therapeutic prospect.
“The concepts of PANoptosomes and PANoptosis are fundamental to our understanding of how innate immune sensing works and can be translated to numerous diseases and conditions,” said Kanneganti. “For conditions with no targeted therapies — inflammatory disorders, infectious disease, cancers, aging — targeting PANoptosis could be an option.”