St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
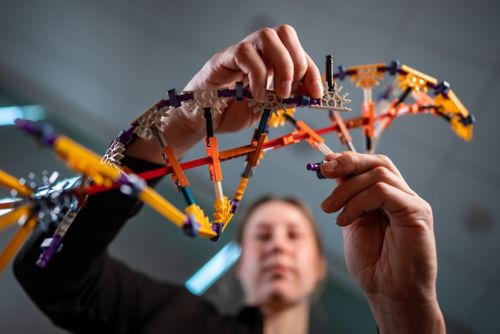
Living things all have needs such as water, sunlight, or nutrients. Tending to the root of health means addressing the foundational factors such, as genetics or the environment, that shape these needs and impact health.
Predicting, preventing and intervening against disease ensures that children at risk of negative health outcomes receive the proper care under the right conditions to thrive. At St. Jude, scientists are studying how to predict who is at risk of disease and which interventions will be most beneficial to prevent diseases from occurring in the first place.

Putting kids first in cancer detection and prevention
Disease detection is entering a golden era where sophisticated classification strategies and genetic screening panels fuel the development of novel detection methods that can lead to better outcomes for patients.
Physicians use this knowledge to tailor targeted treatments to the specific cancer-causing mutations affecting each patient. However, current high-quality whole-genome sequencing requires physical and computational infrastructure that most institutions lack. To address this bottleneck, Xiaotu Ma, PhD, Department of Computational Biology; Jeffery Klco, MD, PhD, Department of Pathology; and John Easton, PhD, Computational Biology Genomics Laboratory director, developed SJPedPanel. Published in Clinical Cancer Research, SJPedPanel is a sequencing platform focusing on genes involved in childhood cancer instead of looking at the entire genome.

SJPedPanel provides the most coverage of pediatric cancer driver genes, providing close to 90% when others are closer to 60% coverage.
Department of Computational Biology
Even though adult cancers are genetically distinct from childhood malignancies, all available genetic screening panels were designed for adult cancers and then adapted for pediatric cancers. St. Jude was one of two institutions that conducted the Pediatric Cancer Genome Project, which sequenced the genomes of 800 patients whose diagnoses included 23 types of cancer to provide the most detailed overview of the genomic landscape of many pediatric cancers. The SJPedPanel covers the risk-related genome regions, occupying just 0.15% of the genome, to provide a comprehensive assay to detect the full spectrum of mutations in pediatric cancers.
“We compared this panel with six commercially available panels,” Ma said. “SJPedPanel provides the most coverage of pediatric cancer driver genes, providing close to 90% when others are closer to 60% coverage.”

Jun J. Yang, PhD, Departments of Pharmacy & Pharmaceutical Sciences and Oncology, examined pediatric and adult B-cell acute lymphoblastic leukemia to assess their differential responses to therapies.
In addition to working better than adapting adult-focused cancer gene panels, the SJPedPanel outperforms gold-standard whole-genome sequencing in some circumstances. Whole-genome sequencing interrogates the entire human genome, making detecting low–cell count cancers difficult.
“There are certain situations, such as low tumor purity samples or even testing after bone marrow transplantation, where current clinical whole-genome sequencing approaches don’t work,” Klco said. “This fills an important clinical gap for our patients.” SJPedPanel is now part of the routine clinical service at St. Jude and will soon be used to monitor patient response during therapy.
The panel will give institutions without resources, such as whole-genome sequencing, a better chance at identifying cancers. “Panels like the SJPedPanel are easier for clinical or research labs to implement than whole-genome sequencing,” Easton said. “Many institutions do not have the sequencing and analysis capabilities to deal with whole-genome data. We’ve given the field a more sensitive and practical test.”
Detecting cancer resistance to prevent the spread of disease
Detecting cancer before it can spread is critical to ensuring overall and long-term health. Even if interventions work on most of a tumor, biological resistance means small populations of cancer cells often survive, and those cells are more challenging to treat. Determining how these robust malignant cells escape treatment is key to true prevention.
The survival of children with relapsed or recurrent ALL is 30%-40%, often due to therapy resistance. In research published in Nature Communications, Daniel Savic, PhD, Department of Pharmacy & Pharmaceutical Sciences, identified and investigated mechanisms behind functional variants within the noncoding region of the genome and explored their contribution to resistance using six drugs that treat leukemia. Despite being devoid of genes, the noncoding region of the genome comprises 98% of DNA and contains a vast number of gene regulatory elements, some of which could contribute to resistance.

We harnessed innovative tools and technologies to systematically examine the noncoding genome and understand its functional effects on ALL pharmacogenomics.
Department of Pharmacy and Pharmaceutical Sciences
By combining massively parallel reporter assays and three-dimensional chromatin looping assays, the St. Jude researchers identified more than 1600 inherited noncoding variants associated with drug resistance in ALL with gene-regulatory roles. This comprehensive study, the largest of its kind to date, prioritized 556 functional noncoding DNA variants that affected gene regulation related to ALL drug resistance in at least three ALL cell lines, identifying a previously unknown resistance mechanism to the chemotherapy drug vincristine. This finding was based on a functional interrogation of the most robust variant, linking its proximity to the gene for EIF3A, a protein involved in cell proliferation and survival, to its resistance mechanism.
“In any genome-wide association study, nearly all associated genetic variants reside in the noncoding genome, so connecting that variation to gene function and an actual trait, such as chemotherapy resistance or disease predisposition, is challenging,” Savic said. “We harnessed innovative tools and technologies to systematically examine the noncoding genome and understand its functional effects on ALL pharmacogenomics. We hope to utilize our findings to improve clinical outcomes in ALL patients.”
Understanding the relationship between genetics and treatment response
Genetics can directly affect how patients respond to treatments and interventions. Acute lymphoblastic leukemia (ALL) affects both children and adults. Children with ALL have a better chance of being cured than adults: long-term survival of childhood ALL exceeds 90%, compared to that of adults, which is 50% to 75%. However, whether ALL has an age-related drug-response profile is unclear. In a study published in the Journal of Clinical Oncology, a team led by Jun J. Yang, PhD, Departments of Pharmacy & Pharmaceutical Sciences and Oncology, examined 767 children and 309 adults with B-cell ALL, assessing the sensitivity of leukemia cells to 21 drugs.
“We found that, for most of the cytotoxic drugs with differential activity between adult and pediatric, it’s largely explained by the age-related differences in the underlying genomic abnormalities of their cancer, namely molecular subtypes,” Yang said.
However, the molecular subtypes of ALL did not explain all the differences in antileukemia drug sensitivity between children and adults however. The researchers found that some children had “adult-like” ALL based on their gene expression profiles, making them more resistant to treatment and leading to poorer outcomes. This finding suggests that age and individual genomics beyond the ALL subtype must be considered to predict treatment response.
“There’s a lot of heterogeneity within each age group,” explained Yang. “You cannot simply divide patients into older than or younger than 18 years and offer therapy based on the legal age of majority; you have to look at their underlying molecular characteristics and pharmacogenomic features.” Together, the group’s findings suggest the need for tailored treatment strategies for both children and adults with B-cell ALL.
Comprehensive data collections, such as the Childhood Cancer Survivor Study and the St. Jude Lifetime Cohort Study, allow scientists to piece together the genetic risks of surviving pediatric cancer.
DNA reveals predisposition in survivors of childhood cancer
Genetic predispositions are found in 5-15% of children with cancer. In a study published in JAMA Oncology, Kim Nichols, MD, Division of Cancer Predisposition director, Department of Oncology, showed that beginning surveillance soon after recognizing a patient’s predisposition often leads to discovering one or more early-stage asymptomatic tumors, most of which could be removed after chemotherapy and/or radiation therapy, and about half of which could be removed surgically.
The researchers examined 274 pediatric patients at St. Jude who carried 35 different cancer-predisposing syndromes over a median of three years. Surveillance revealed 35 tumors in 27 patients, representing a broad array of solid and central nervous system cancers. This group included a subset of about 17% of children who had a new tumor identified while they were still undergoing treatment for a prior cancer. This finding suggests providers should not wait until a child has finished treatment for their first cancer before they start screening for other potential malignancies.

Understanding whether children have an underlying genetic risk for cancer can greatly impact their clinical care. Proactive surveillance for new tumors is an important component of this care.
Department of Oncology
To find potential cancers and guide treatment, clinicians used various surveillance methods. For example, a predisposition for a solid tumor may lead to annual full-body magnetic resonance imaging (MRI). Standard surveillance methods had minuscule false positive and false negative rates. “We’ve shown that standardized surveillance protocols provide a very effective way to detect new tumors at their earliest and most treatable stages,” Nichols said. “Understanding whether children have an underlying genetic risk for cancer can greatly impact their clinical care. Proactive surveillance for new tumors is an important component of this care.”
The study may enable more providers to order these effective, yet sometimes expensive, tests. It can be challenging for providers to get insurance companies to pay for early screening. Historically, this has created a difficult cycle where providers could not order the tests, which meant there was no strong evidence of their value, preventing their use. Patients at St. Jude are treated regardless of insurance coverage, thus enabling physicians to order the appropriate tests. The excellent performance of the standard screening methods is evidence that early testing can improve detection and outcomes. This may give insurance companies the evidence needed to cover the tests for children with a predisposition.
Avoiding long-term effects of cancer on health
Cancer has life-long effects. Survivorship research focuses, in part, on predicting and preventing these long-term adverse effects. Published in the Journal of Clinical Oncology, a study led by Yadav Sapkota, PhD, Department of Epidemiology & Cancer Control, identified four previously unknown genetic variants associated with diabetes risk in childhood cancer survivors. Furthermore, the genetic risks for diabetes appeared to be not only magnified by childhood exposure to alkylating agents (a common class of chemotherapeutics) but also exacerbated by ancestry.
“The genetic risk disproportionately affected survivors of African or African American ancestry previously treated with alkylating agents,” Sapkota said. “The same variant is implicated in both European and African-ancestry groups, but the amount of risk conferred by carrying the variant differs.”

Now we know how to identify childhood cancer survivors most at risk of diabetes so we can provide more personalized opportunities for interventions and prevent cardiovascular complications down the road.
Department of Epidemiology & Cancer Control
In addition to individual genetic variants, combinations of many genetic variants previously associated with diabetes risk in the general population, considered as a score, have been studied to assess disease risk in childhood cancer survivors. However, these scores have been derived typically from studies involving only individuals of European descent. Thus, the researchers compared three scores: one based on those of European descent only and two others developed by including individuals of different ancestries. The more inclusive scores more accurately predicted diabetes risk in survivors of both European and African ancestries.
“We hope this information will help reduce differences in the diabetes burden,” Sapkota said. “Now we know how to identify childhood cancer survivors most at risk of diabetes, so we can provide more personalized opportunities for interventions and prevent cardiovascular complications down the road.”
Minimizing symptom burden to maximize quality of life
While detecting disease risk is at the root of improving clinical outcomes, long-term monitoring is required for quality-of-life improvements to endure. Treatment for medulloblastoma, a type of childhood brain tumor, is associated with neurocognitive impairments. The outlook for patients with medulloblastoma has improved over time. However, Tara Brinkman, PhD, Departments of Psychology & Biobehavioral Sciences and Epidemiology & Cancer Control, and her colleagues showed in research published in Neuro-Oncology that the risk of neurocognitive impairment remains a concern.
The researchers surveyed 505 survivors of medulloblastoma from the Childhood Cancer Survivor Study (CCSS), a multi-institution retrospective cohort with prospective follow-up led by Gregory Armstrong, MD, MSCE, Department of Epidemiology & Cancer Control chair. They categorized the participants based on the treatment received.

Routine surveillance of neurocognitive functioning in survivors remains critical to understanding the long-term effects of contemporary therapies.
Departments of Psychology & Biobehavioral Sciences and Epidemiology & Cancer Control
Childhood medulloblastoma survivors who were treated between 1970 and 1999 experienced as much as a five-fold increased risk of cognitive deficits compared to that of their healthy siblings. Notably, the researchers observed that the survivors’ ability to achieve independence in adulthood is adversely impacted by the development of neurocognitive problems and chronic health conditions after treatment for medulloblastoma.
“Routine surveillance of neurocognitive functioning in survivors remains critical to understanding the long-term effects of contemporary therapies,” Brinkman said. “Surveillance efforts further inform our ability to prevent and manage disease and treatment-related late effects to optimize quality of life.”
In addition to how clinical factors affect patient outcomes, research on how contextual factors such as low socioeconomic status, unstable housing, and transportation barriers affect the health of childhood cancer survivors mainly focused on those survivors who reached adulthood. This approach has left a gap in understanding the experiences of children and adolescents at least five years post-diagnosis and younger than 18 years.

St. Jude investigator I-Chan Huang, PhD, is leading research using wearable devices that track variables such as heart rate, helping gather important data about the health of childhood cancer survivors.
Published in JAMA Network Open, a study from I-Chan Huang, PhD, Department of Epidemiology & Cancer Control, examined the physical and psychological symptoms in children and adolescents aged 8 to 18 years and explored the contextual factors’ impacts. This involved identifying associations with sociodemographic, clinical, and psychological resilience skills and health-related quality of life. The study provides a comprehensive portrait of the challenges faced by young survivors and suggests ways to develop targeted interventions.
By examining contextual factors in 302 young childhood cancer survivors, the investigators found that nearly 40% of the cohort self-reported moderate or high cumulative overall symptom burden. Factors that correlated strongly with symptom burden included caregiver anxiety and neighborhood deprivation, which cover aspects such as income and living environment. “If parents have anxiety, there is almost a two-fold higher risk that survivors will have a higher symptom burden,” Huang explained. This conclusion is compounded by evidence showing that children living in high-vulnerability neighborhoods have a five-fold higher risk of experiencing high symptom burden.

I want to see the dynamics of the symptoms and how they evolve over time.
Department of Epidemiology & Cancer Control
The study identified preventative factors that can mitigate symptom burden. For example, “We found the association between parents’ anxiety and the survivor’s disease burden decreases with high levels of survivor resilience,” said Huang. A sense of resilience reduced the impact of negative contextual factors on symptom burden by 30% to 40%.
However, while the survivor’s resilience can mitigate personal and family issues, community factors need broader solutions. “We need to find a way to identify and screen for the origin of their symptoms, then provide the necessary intervention,” Huang said.
Patient-reported outcomes are a key metric to understanding symptom burden, but clinicians are limited by the frequency of assessments — often only once every couple of years. “I don’t believe using these snapshots to understand symptom burden is enough,” Huang said. “I want to see the dynamics of the symptoms and how they evolve over time.”
In a pilot study of 41 participants published in Cancers and a larger study protocol involving 600 survivors described in Frontiers in Oncology, Huang explored utilizing mobile health technology (mHealth) to achieve this. The researchers collected daily symptom data, momentary digital biomarkers (e.g., heart rate variability, respiratory rate, skin temperature, etc.), and overall progression of late effects over five years. The mobile platform enabled the researchers to send symptom and quality-of-life surveys to participants daily, which prompted them to report on 20 symptoms. They also tracked digital biomarkers through wearable activity monitors.
The researchers noted that some symptoms remained stable, but many demonstrated high variability from day to day, month to month, and even between individuals. “It suggests that we need more frequent symptom assessments rather than relying on yearly or less frequent clinic visits,” said Huang. “This also means that intervention strategies should be tailored to account for this variability.”
To collect robust data, using wearable devices represents a key feature of the study to Huang. “Combining wearable device data, such as heart rate, activity levels, and sleep patterns, with self-reported symptom data allows us to identify patterns,” Huang said. “We can then predict various disease progression outcomes and integrate this prediction algorithm into the clinical workflow as a key component of the clinical warning system for managing late effects.”

Epidemiological research investigates the distribution patterns and determinants of health and disease conditions in specific populations, which can be applied to help predict and prevent disease
Providing a blueprint for prediction and prevention
While there is no exact blueprint for human health that will tell providers exactly who is at risk of disease or how to treat them – scientists are working to fill in gaps in knowledge, giving providers clues about the factors that influence health and how they can be assessed, modified, and used to tailor care for each person. A vast array of factors shape a person’s health, and with the right interventions, challenges can be overcome. Just as a plant with proper care can flourish despite harsh conditions, children can thrive when the root factors that shape their healthcare outcomes are understood.